Antimicrobial resistance patterns of Enterobacterales isolated from 2018 to 2020, Medilab Clinic – Medihospital, Loja
DOI:
https://doi.org/10.54753/cedamaz.v14i1.1850Keywords:
Enterobacteria, Bacterial drug resistance, Escherichia coli, Klebsiella pneumoniaeAbstract
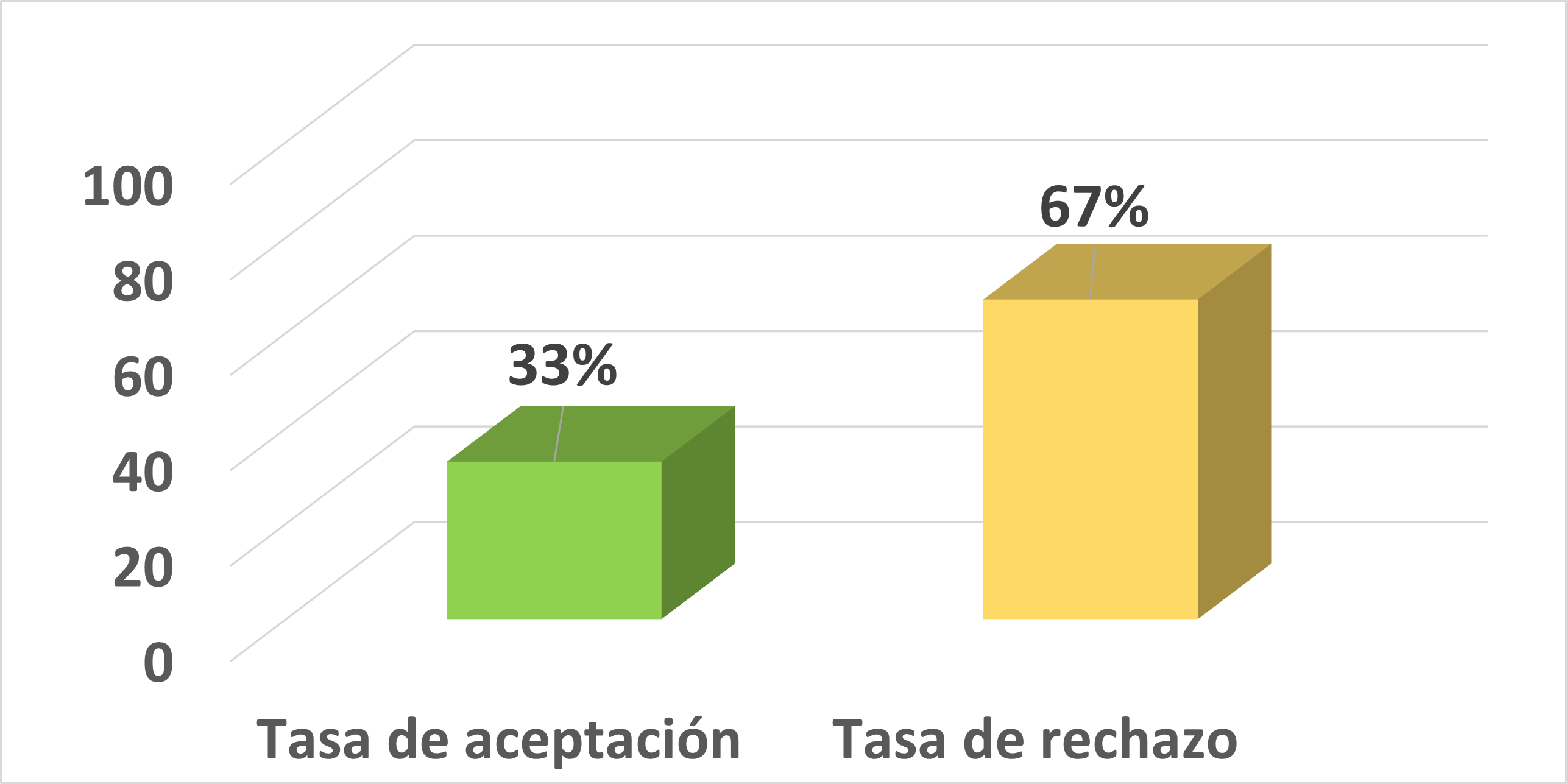
Among the factors that favor the appearance of bacterial resistance is the continuous exposure to drugs, which allows bacteria to adapt and mutate, avoiding their lysis and maintaining their growth capacity, limiting the use of antibiotic therapy for their eradication, which causes the need to create new drugs for the treatment of these "superbacteria", therefore, knowing the antimicrobial susceptibility patterns of the circulating strains in the environment allows to make right medical decisions for an empirical treatment. The present research work had a quantitative approach and a retrospective-cross-sectional design. The objective was to determine the patterns of antimicrobial resistance of Enterobacterales in samples of patients from hospitalization and outpatient clinic who attended the Medilab Clinic – Medihospital in the period 2018 - 2020. The study included 848 reports of crops and antibiograms whose isolates identified Enterobacterales; urine represented 90,21% of the samples processed, Escherichia coli was the prevalent pathogen in urine, blood and secretions with 83%, 80% and 33,90% respectively. According to the antimicrobial resistance pattern of hospital strains, Klebsiella pneumoniae had resistance percentages greater than 70% for nitrofurantoin, amoxicillin/clavulanic acid, and first and third generation cephalosporins, the 34,39% was ESBL and the 9,76% carbapenemases; maintained its sensitivity to carbapenems, while Enterobacter cloacae in community strains, presented percentages of 100% resistance against second, third and fourth generation cephalosporinsReferences
Asamoah, B., Labi, A., Gupte, H., Davtyan, H., Peprah, G., Adu-Gyan, F., . . . Nyantakyi, P. (2022). High Resistance to Antibiotics Recommended in Standard Treatment Guidelines in Ghana: A Cross-Sectional Study of Antimicrobial Resistance Patterns in Patients with Urinary Tract Infections between 2017–2021. International Journal of Environmental Research and Public Health, 19. doi:https://doi.org/10.3390/ijerph192416556
Bathia, R. (2018). Resistencia a los antimicrobianos: amenaza, consecuencias y opciones. The National Medical Journal of India, 31. doi:10.4103/0970-258X.255752
Betrán, A., Lavilla, M., Cebollada, R., Calderón, J., & Torres, L. (2020). Resistencia antibiótica de Escherichia coli en infecciones urinarias nosocomiales y adquiridas en la comunidad del Sector Sanitario de Huesca 2016-2018. Revista Clínica de Medicina de Familia, 13. Obtenido dehttp://bitly.ws/Cktx Camacho, L. (2023). Resistencia bacteriana, una crisis actual. Rev Esp Salud Pública, 97. Obtenido de https://medes.com/publication/176098
Della Rocca, M., Panetta, V., Durante, A., Bucci, L., Matano, A., Annecchiarico, A., & Greco, R. (2022). Pathogens distribution and antimicrobial resistance pattern of blood stream infections in Southern Italian hospital, 2016-2021 surveillance. New Microbiologica, 46.
Espinoza, C., Cando, V., & Acosta, L. (2020). Resistencia antimicrobiana de enterobacterias y uso de antibióticos en pacientes de uci clínica Dame 2014. Polo del Conocimiento, 5. doi:https://doi.org/10.23857/pc.v5i4.1379
Gentil, P., Canton, R., López, V., Barberán, J., Blasco, A., Gutierrez, C., . . . Horcajada, J. (2022). Antimicrobial resistance in Gram-negative bacilli in Spain: an experts’ view. Revista Española de Quimioterapia, 36. Gonzalez, J., Maguiña, C., & González, F. (2019). La resistencia a los antibióticos: un problema muy serio. Acta Médica Peruana, 36. Obtenido de http://bitly.ws/Cvnr
Gordillo, F., & Barrera, F. (2018). Perfil de resistencia de uropatógenos en pacientes con diabetes en Quito, Ecuador, inquietante panorama. Enfermedades Infecciosas, 60. doi:https://doi.org/10.21149/8756
Jimenez, G., Morejón, M., & Ramón, S. (2022). Agentes etiológicos de las bacteriemias en el área de salud de Ibiza y Formentera (ASEF) durante el año 2019. Revista Sanitaria de Investigación, 11. Obtenido de http://bitly.ws/CvWT
Kenneth, R., & George, R. (2017). Sherris. Microbiología Médica. Obtenido de http://bitly.ws/CvWj
Lepe, J., & Martinez, L. (2022). Mecanismos de resistencia en bacterias gramnegativas. Medicina Intensiva, 46. doi:https://doi.org/10.1016/j.medin.2022.02.004
Ljungquist, O., Blomstergren, A., Merkel, A., Sunnehagen, T., Holm, K., & Torisson, G. (2022). Incidence, aetiology and temporal trend of bloodstream infections in southern Sweden from 2006 to 2019: a population-based study. Revista europea sobre vigilancia, epidemiología, prevención y control de enfermedades infecciosas, 28. doi:https://doi.org/10.2807/1560-7917.ES.2023.28.10.2200519
Morales, A., Sánchez, F., Agreda, I., Maldonado, C., Morales, L., Gallegos, M., Arias, R., Chango, F., Estrada, E., Andrade, J., Jaramillo, C., & Pichucho, B. (2021). Patrones de resistencia bacteriana en la Unidad de Cuidados Intensivos del Hospital General Ambato del IESS, Ecuador. Archivos Venezolanos de Farmacología y Terapéutica. doi:https://doi.org/10.5281/zenodo.4676295
Morales, R., Contreras, I., Duran, A., Olivares, A., Valencia, C., García, Y., & González, A. (2020). Patrones de susceptibilidad antimicrobiana “in vitro” de bacterias Gram negatives asilades de infección de vías urinarias en pacientes ambulatorios de una clínica del sur de la Ciudad de México. Obtenido de https://bitly.cx/t8EP
Parker, J., Gu, R., Estrera, G., Kirkpatrick, B., Ros, D., Mavridou, D., . . . Davies, B. (2023). Carbapenem-Resistant and ESBL-Producing Enterobacterales Emerging in Central Texas. Infection and Drug Resistance, 16. doi:https://doi.org/10.2147/IDR.S403448
Pascual, P., Cantero, M., Muñez, E., Asensio, A., & Ramos, A. (2020). Epidemiología y clínica de las infecciones y colonizaciones causadas por enterobacterias productoras de carbapenemasas en un hospital de tercer nivel. Revista Española de Quimioterapia, 33, 112-129. Obtenido de http://bitly.ws/CvWy
Sajona, E., Osorio, E., & Peña, L. (2018). Perfil de resistencia de escherichia coli en infecciones del tracto urinario (ITU), en pacientes de consulta externa de la fundación hospital universitario metropolitano de barranquilla. Revista Edu-fisica, 10. Obtenido de http://bitly.ws/CvT6
Salame, L., Contreras, B., Arias, S., Mondragón, M., Cataneo, J., Núñez, M., & Valente, B. (2018). Epidemiología de las bacteriemias por Escherichia coli en dos hospitales de tercer nivel de la Ciudad de México. Medigraphic, 63. Obtenido de http://bitly.ws/Cvnc
Shields, R., Zhou, Y., Kanakamed, H., & Cai, B. (2021). Burden of illness in US hospitals due to carbapenemresistant Gram-negative urinary tract infections in patients with or without bacteraemia. BMC Infectious Diseases, 21. doi:https://doi.org/10.1186/s12879-021-06229-x
Toombs, L., Marshall, J., Benschop, J., Drinkovi, D., Midwinter, A., Bigg, P., . . . Burgess, S. (2022). Extendedspectrum β-lactamase- and AmpC β-lactamase-producing Enterobacterales associated with urinary tract infections in the New Zealand community: a case-control study. International Journal of Infectious Diseases, 128. doi:https://doi.org/10.1016/j.ijid.2022.12.013
Valery, F., Salgado, J., Rosal, E., Reyes, M., & Moreno, C. (2016). Evaluación de la resistencia bacteriana en el Hospital Pediátrico “Dr. Elías Toro”. Años 2012 al 2016. Recomendaciones prácticas. Infectologia. Revista Bol Venez Infectología, 27. Obtenido de http://bitly.ws/CvSn
Yoshimura, J., Yamakawa, K., Umemura, Y., Nishida, T., Ooi, Y., & Fujim, S. (2021). Impact of beta-lactamase detection reagent on rapid diagnosis of ESBL-producing pathogens using urine samples of patients with Gramnegative bacteriuria. International Journal of Infectious Diseases, 113. doi:https://doi .org/10 .1016/j .ijid.2021.09.059
Zhang, H., Xu, J., Xiao, Q., Wang, Y., Wang, J., Zhu, M., & Cai, Y. (2023). Carbapenem-sparing beta-lactam/betalactamase inhibitors versus carbapenems for bloodstream infections caused by extended-spectrum beta-lactamaseproducing Enterobacteriaceae: a systematic review and meta-analysis. International Journal of Infectious Diseases, 128. doi:https://doi.org/10.1016/j.ijid.2023.01.001
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 CEDAMAZ

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Those authors who have publications with this journal, accept the following terms:
- After the scientific article is accepted for publication, the author agrees to transfer the rights of the first publication to the CEDAMAZ Journal, but the authors retain the copyright. The total or partial reproduction of the published texts is allowed as long as it is not for profit. When the total or partial reproduction of scientific articles accepted and published in the CEDAMAZ Journal is carried out, the complete source and the electronic address of the publication must be cited.
- Scientific articles accepted and published in the CEDAMAZ journal may be deposited by the authors in their entirety in any repository without commercial purposes.
- Authors should not distribute accepted scientific articles that have not yet been officially published by CEDAMAZ. Failure to comply with this rule will result in the rejection of the scientific article.
- The publication of your work will be simultaneously subject to the Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)