Conversión bacteriológica asociada a co-morbilidad y prestación de servicios, en casos nuevos de Tuberculosis Pulmonar BK+. Zona 7 Ecuador
Palabras clave:
Conversión bacteriológica, diabetes y tuberculosisResumen
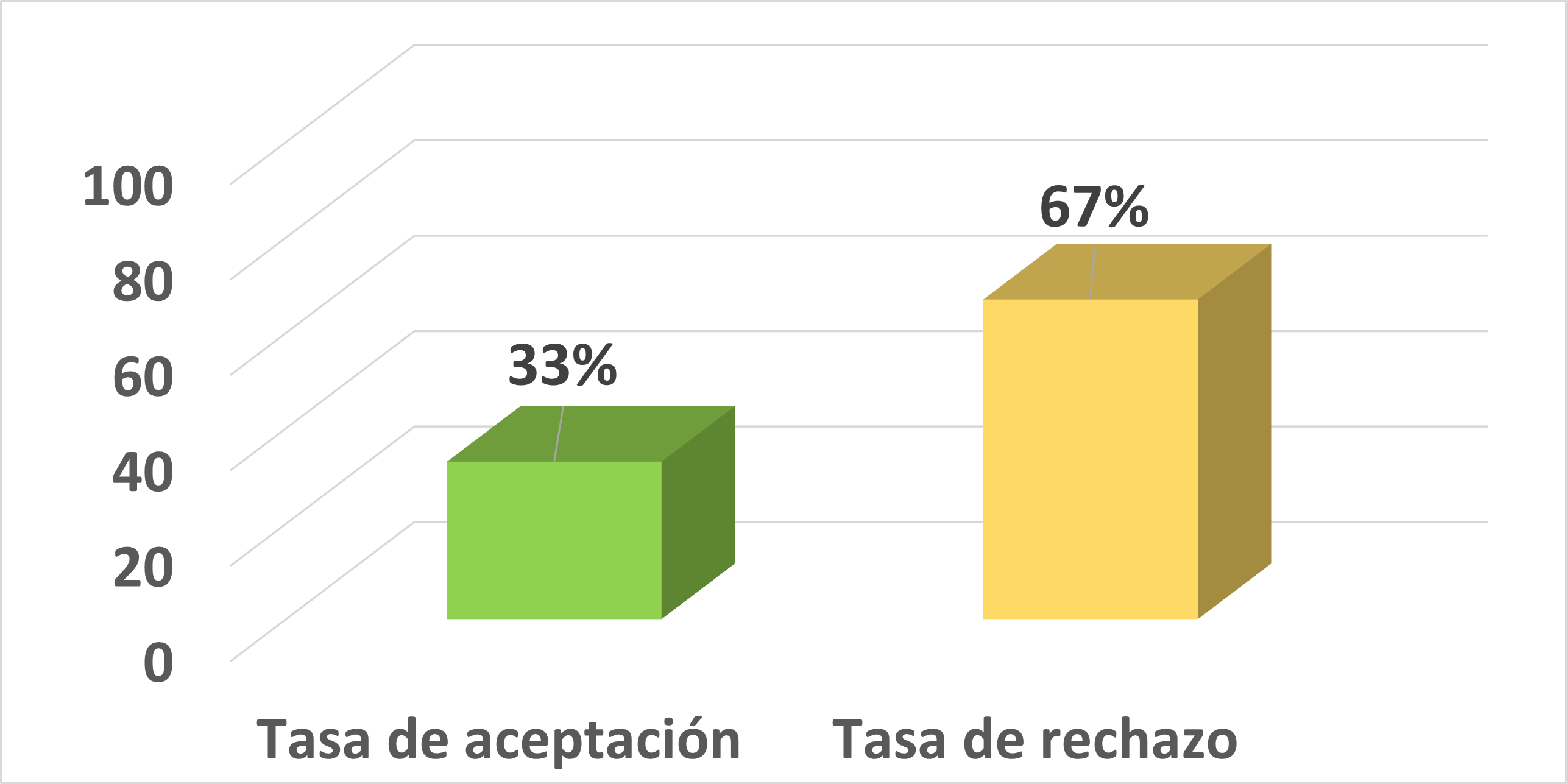
La tuberculosis es un problema de salud pública que sigue afectando al mundo, de manera particular a los países más pobres y en vías de desarrollo; Ecuador se encuentra en el sexto lugar de prevalencia de Tb en las Américas; la provincia de El Oro ubicada en la Zona Siete es una de las más afectadas; en la misma se han reportado casos de no conversión bacteriológica y se desconocen los factores que están incidiendo. El estudio se orientó a estimar el tiempo de negativización bacteriológica en casos nuevos con tuberculosis pulmonar BK+ positivos y su probable asociación a comorbilidad y prestación de servicios. Este estudio de diseño correlacional y prospectivo se desarrolló en la Zona Siete, durante el período de 2013-2015; la población estuvo integrada por 389 casos nuevos diagnosticados por baciloscopía. Los resultados de conversión bacteriológica al segundo mes de tratamiento fue 91,70 %; los factores asociados a la no conversión son: sexo masculino (OR= 5,58 IC95 %= 1,92-16,24 p =0,00), carga bacilar >= ++ (OR= 3,87 IC95 % =1,55-9,63 p= 0,02) y diabetes (OR= 2,51 IC95 %= 1,15-5,51 p= 001). En conclusión, la conversión bacteriológica al segundo mes de tratamiento no se logra en el 100 % de los casos en la Zona Siete del Ecuador y los factores asociados son sexo masculino, carga bacilar >= ++ y la diabetes.Citas
Asalde, C.B., 2008. Situación de la Tuberculosis en el Perú. , 25(3), pp. 163–170.
Bawri, S. et al., 2008. A study of sputum conversion in new smear positive pulmonary tuberculosis cases at the monthly intervals of 1, 2 & 3 month under directly observed treatment, short course (dots) regimen. Lung India : of cial organ of Indian Chest Society, 25(3), pp. 118–23. Available at: http://www. pubmedcentral.nih.gov/articlerender.fcgi?artid =2822329&tool=pmcentrez&rendertype=abst ract [Accessed October 17, 2012].
Caetano Mota, P. et al., 2012. Predictors of delayed sputum smear and culture conversion among a Portuguese population with pulmonary tuberculosis. Revista portuguesa de pneumologia, 18(2), pp.72–9. Available at: http://www.ncbi.nlm.nih.gov/ pubmed/22277838 [Accessed October 4, 2012].
D’Alessandro, A., Mogollón, C. & Waard, J., 2008. Baciloscopia positiva persistente en fase avanzada de la terapia anti- tuberculosa: No siempre indica fracaso del tratamiento. Revista chilena de Infect 2008, 25(3), pp.209–212. Available at: http://www.scielo.cl/scielo.php?pid=S0716- 10182008000300014&script=sci_arttext [Accessed October 9, 2012].
Dooley, K.E. et al., 2009. Impact of diabetes mellitus on treatment outcomes of patients with active tuberculosis. The American journal of tropical medicine and hygiene, 80(4), pp.634– 639. Available at: http://www.pubmedcentral. nih.gov/articlerender.fcgi?artid=2750857&too l=pmcentrez&rendertype=abstract [Accessed October 4, 2012].
Gomez, P. et al., 2009. Evaluación de los indicadores epidemiológicos del programa de Tuberculosis. Matanzas. Años 2002/2006. Revista Médica Electrónica, Centro Provincial Higiene y epidemiología, Matanzas, 31(2), p. 13.
Gullón Blanco, J.A. et al., 2007. Tabaquismo y negativización bacteriológica del esputo en la tuberculosis pulmonar. Medicina Clínica, 128, pp.565–568.
Van Helden, P.D. et al., 2012. TUBERCULOSIS (TB) Y DIABETES MELLITUS (DM) EN EL PRIMER NIVEL DE ATENCIÓN. , 8(Dm), p.45.
Heredia, N.S. & Lezama, M. a S., 2011. Tuberculosis y diabetes mellitus en la jurisdicción sanitaria número 2 del estado de guerrero. una comunicación breve de un estudio descriptivo. Revista del Instituto Nacional de Enfermedades Respiratorias,70(3), pp. 152–156.
Maciel, E.L.N. et al., 2013. Smoking and 2-month culture conversion during anti- tuberculosis treatment. International Journal of Tuberculosis and Lung Disease, 17(September 2012), pp.225–228.
Martínez-Medina, M.A., 2004. Efecto del tratamiento acortado estrictamente supervisado ( TAES ) sobre la adherencia y la tasa de curación de la tuberculosis pulmonar. Gaceta Médica de México, 140(1), p.7. Available at: pesquisa.bvsalud.org/regional/ resources/lil-632141.
Ministerio de Salud de la Nación de Argentina, 2013. Programa Nacional de Control de la Tuberculosis. Normas Técnicas 2013, Argentina.
MSP Ecuador, 2010. Manual de Normas y Procedimientos para el Control de la Tuberculosis Ecuador 2da. ed., Quito-Ecuador.
Ozsahin, S. & Arslan, S., 2011. Chest X-ray and bacteriology in the initial phase of treatment of 800 male patients with pulmonary tuberculosis. Jornal Brasileiro de ..., 37(3), pp.294–301. Available at: http://www.scielo.br/scielo.php?pid=S1806- 37132011000300004&script=sci_ arttext&tlng=es [Accessed September 18, 2014].
Park, S.W. et al., 2012. The effect of diabetic control status on the clinical features of pulmonary tuberculosis. European journal of clinical microbiology & infectious diseases : of cial publication of the European Society of Clinical Microbiology, 31(7), pp. 1305–10. Available at: http://www.ncbi.nlm.nih.gov/ pubmed/22042559 [Accessed October 4, 2012].
Pilheu, J.A. et al., 2002. Tratamiento directamente observado, semanal, en tuberculosis: estudio prospectivo en Buenos Aires, Argentina/ Treatment directly observed, weekly, in tuberculosis: Prospective study in Buenos Aires, Argentina. Available at: http://pesquisa. bvsalud.org/regional/resources/lil-333222 [Accessed October 17, 2012].
Senkoro, M., M nanga, S.G. & Mørkve, O., 2010. Smear microscopy and culture conversion rates among smear positive pulmonary tuberculosis
patients by HIV status in Dar es Salaam, Tanzania. BMC infectious diseases, 10, p.210. Available at: http://www.pubmedcentral.nih. gov/articlerender.fcgi?artid=2918607&tool=p mcentrez&rendertype=abstract.
SENPLADES, 2010. AGENDA ZONAL PARA EL BUEN VIVIR: Propuestas de Desarrollo y Lineamientos para el Ordenamiento Territorial, Loja. Available at: http://www.pnud.org.ec/art/ frontEnd/images/objetos/agenda_7.pdf.
Siddiqui, U.A. et al., 2010. Smoking prolongs the infectivity of patients with tuberculosis. Irish medical journal, 103(9), pp.278–80. Available at: http://www.ncbi.nlm.nih.gov/ pubmed/21186753 [Accessed October 4, 2012].
SISTEMA NACIONAL DE INFORMACIÓN, 2012. PROYECCIONES DE POBLACIÓN.
Stoffel, C. et al., 2014. TRATAMIENTO DE LA TUBERCULOSIS PULMONAR EN UN ÁREA URBANA DE BAJA PREVALENCIA . CUMPLIMIENTO Y NEGATIVIZACIÓN BACTERIOLÓGICA Materiales y métodos. Medicina Buenos Aires, 74, pp.9–18.
Suhadev, M. et al., 2011. Alcohol use disorders (AUD) among tuberculosis patients: a study from Chennai, South India. PloS one, 6(5), p.e19485. Available at: http://www. pubmedcentral.nih.gov/articlerender.fcgi?artid =3096635&tool=pmcentrez&rendertype=abst ract [Accessed October 17, 2012].
Toman, K., 2007. Tuberculosis: detección de casos, tratamiento y vigilancia. Preguntas y respuestas. Cadernos de Saúde Pública, 23(617), pp.2519–2520.
Tuesta Soldevilla, J., 2014. Nuestra experiencia en el tratamiento acortado de la tuberculosis / Our experience in the brief treatment of tuberculosis. Portal de Pesquisa da BVS, 18(2).
Word Healt Organization, 2013. De niciones y marco de trabajo para la noti cación de Tuberculosis – Revisión 2013,
Worl Health Organization, 2015. Global Tuberculosis Report 2014, Key indicators for the WHO Region of the Americas Estimates,
Worl Health Organization, 2014. Reporte Global de la Tuberculosis. Revista de la OMS.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
-
Luego que el artículo científico es aceptado, para su publicación el o la autora aceptan ceder los derechos de la primera publicación a la Revista CEDAMAZ, conservando sus derechos de autor. Se permite la reproducción total o parcial de los textos que se publican siempre y cuando sea sin fines de lucro. Cuando se ejecute la reproducción total o parcial de los artículos científicos aceptados y publicados en la revista CEDAMAZ, se debe citar la fuente completa y la dirección electrónica de la publicación.
-
Los artículos científicos aceptados y publicados en la revista CEDAMAZ pueden ser depositados por los autores de manera integra en cualquier repositorio sin fines comerciales.
-
Los autores no deben distribuir los artículos científicos aceptados, pero que todavía no han sido publicados oficialmente por la revista CEDAMAZ. En el caso de incumplir esta norma implica el rechazo del articulo científico.
- La publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons